

Introduction
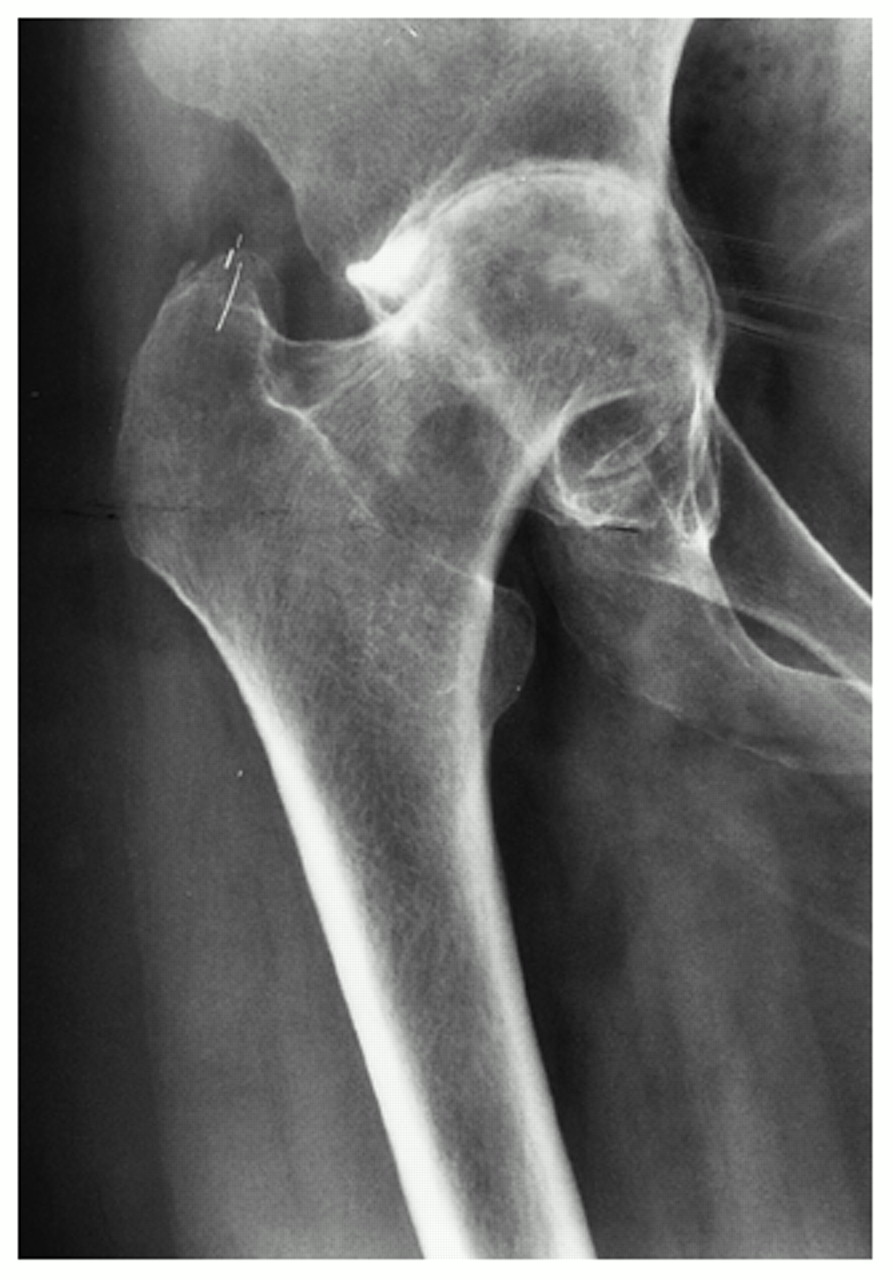
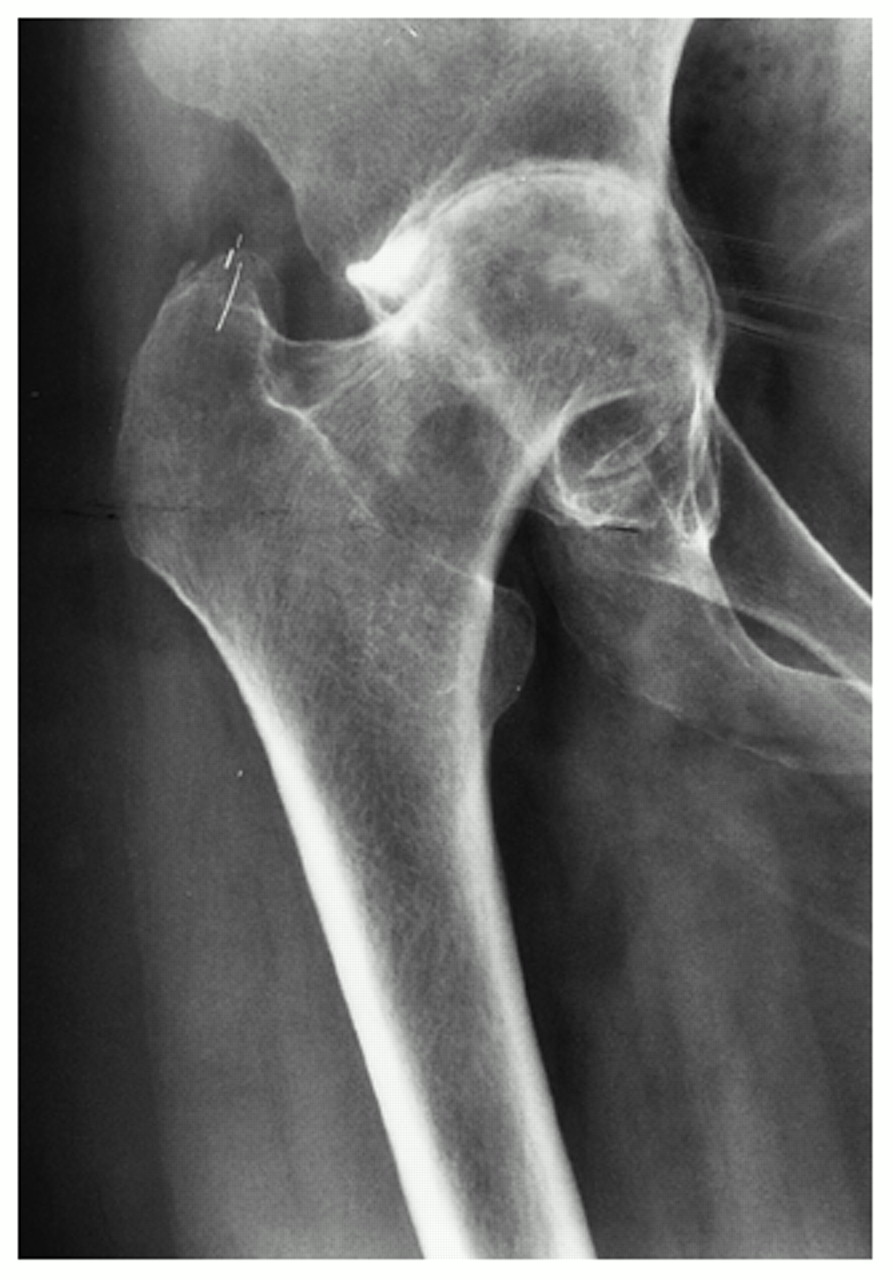
Rheumatic arthritis causes joint erosion and joint destruction visible on x-rays and symptoms that can be severe and limiting. As the joint becomes eroded the cartilage is damaged and the articulation of bone-on-bone causes severe pain. Damage to cartilage, tendons, ligaments and bone causes the hip joint to become deformed and even unstable as rheumatoid arthritis progresses.
Special considerations
Patients with rheumatoid arthritis often have multiple joint problems, simply replacing the hip may not bring as much benefit as we would expect if this was the only diseased joint. However these hip joints can become very disabling and hip replacement should not be withheld or delayed simply because of the associated problems.
All intra-capsular femoral neck fractures in patients with rheumatoid arthritis should be treated with a total hip replacement, there is no place for hemiarthroplasty. Rheumatoid patients require immediate weight bearing and maximum stability, avoid uncemented stems or any technique requiring partial weight-bearing.
The frequency of acetabular protrusio is higher in rheumatoid hips as is the likelihood of significant femoral head deformity. Bone quality is poor especially in those patients who have needed long term steroid treatment. This makes these operations more difficult, with a higher risk of per-operative and post-operative complications.
Infection is slightly more common in patients with rheumatoid arthritis, partly due to the disease and partly due to the drugs used for treatment. As the soft tissues are affected by the rheumatoid process the risk of post-operative limp is higher, along with the rate of hip dislocation.
© Mr Gavin Holt :: CotswoldClinics.com :: Print this frame