Introduction
Osteoarthritis is the term used for worn out joints and the hip is a common site for symptoms. This is a weight bearing joint and therefore once the joint starts to fail, it will progressively deteriorate.
Aetiology
There are many factors contributing to early failure of the hip joint, most are asymptomatic until the fourth or fifth decade (explaining the failure of natural selection to rid us of hip arthritis!). In any mechanical joint the longevity relates to three key features: -
Abnormally shaped hips are prone to wear early in life and then develop osteoarthritis. Many conditions from childhood can lead to abnormal shaped hips in adults. For a very few patients interventions in adolescence may be appropriate to make the hip more normal and delay the onset of osteoarthritis. Most patients are unaware of small abnormalities of their hips until osteoarthritis develops. As these small abnormalities are not amenable to treatment there is no place for screening followed by "early" treatment.
There is controversy surrounding the influence of treatment for labral tears and impingement, on the future development of osteoarthritis.
The articular cartilage of the hip has evolved to use very low friction "elastohydrodynamic" lubrication. As with all tissues in the body some patients have better cartilage than others, and this is reflected in the inherited risk of hip replacement. Any damage to the articular cartilage is likely to lead to accelerated wear. This is common after intra-articular acetabular or femoral head fractures and also after septic arthritis of the hip.
Load across the hip joint can reach seven times bodyweight during walking. Put another way every 2 lbs of excess weight round the stomach adds a stone to the load across the hip joint. Normal adults take 4 million steps a year and although the joint has some reparative potential the wear is accumulative. Running and jumping cause very high peak loads on the hip joint and will test the hips ability to repair itself. Any training with added weight puts very high repeated forces on the hip joint e.g. TAB with a 35 - 55 lbs Bergen!
Classification
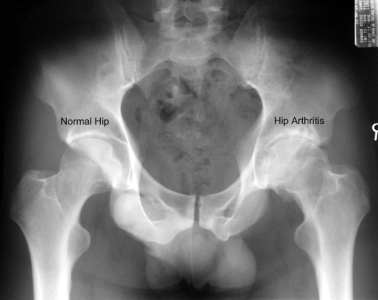
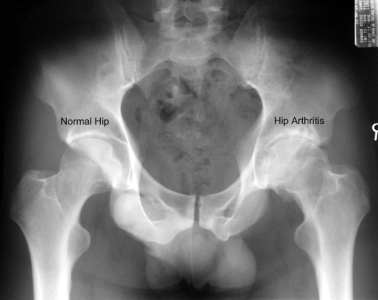
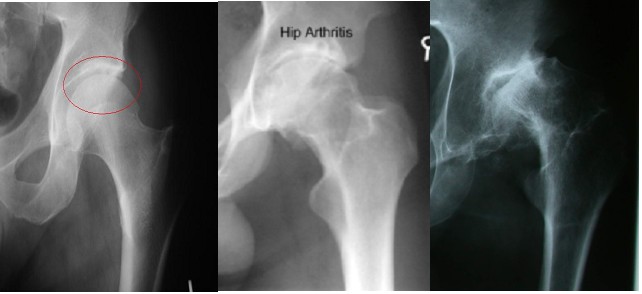
Standing x-rays of the hip joint will give a good assessment of remaining joint space and bone changes related to arthritis:
Tönnis Classification:
The articular surfaces of the hip can be assessed by contrast MRI arthrography[1]. However there is no widely accepted system for MRI grading of chondral loss in the hip joint. Many have used a modification of the Outerbridge classification and applied to named parts of the joint. In the future a system based upon the percentage volume of lost cartilage may be most appropriate.
Inspection of the joint surfaces by arthroscopy or open surgery allows grading using established classifications:
Outerbridge Classification:
As an aid to decision making in treating hip pathology the joint specific grading of Beck [2] may be more useful:
Beck Classification:
Diagnosis
Patients usually present with a gradual onset of hip in the groin. They may note stiffness, difficulty get down to the toenails or with socks/stockings. Loss of rotational movement is the cardinal sign on examination. This is tested in extension "rolling the leg on the couch" and in flexion "twisting the hip using the tibia as a lever". In the early stages the movement may be present, but limited by "end of range pain".
As the condition progresses the stiffness or pain may induce a limp. Night pain becomes more prominent and sleeping is disturbed. In advanced cases the leg may be fixed in flexion and adduction - producing apparent leg lengthening. A small number of patients will develop a secondary AVN with
A simple x-ray should show changes of osteoarthritis. The x-ray findings classically include as joint space narrowing, subarticular sclerosis, osteophytes and degenerative cyst formation.
Patients presenting at a young age are often told they have a groin strain and x-rays are not undertaken - delaying the diagnosis. If x-rays are normal an alternative diagnosis should be sort.
Treatment
There are no proven interventions to halt the progression of osteoarthritis once established. The severity and progression of symptoms can be reduced by weight-loss and physiotherapy mobilizations. The impact of symptoms upon quality of life can be reduced by the regular pain killing medications and the use of a walking stick or pole.
The mainstay of treatment for hip arthritis is total hip replacement, this description covers all operations where two artificial surfaces articulate to recreate pain free hip movement. There are many types of total hip replacement and a large industry of suppliers trying to promote their latest (and most expensive) products. The results of total hip replacement are bested assessed by the number of implants surviving more than 10 years, therefore it takes considerable time to fully evaluate any new design - newer is not always better.
In the Teaching Zone here is a section on total hip replacement which covers the indications, technologies (including resurfacing and ceramic joints) techniques and results.
© Mr Gavin Holt :: CotswoldClinics.com :: Print this frame