|
|
Introduction
This term is used for AVN of unknown cause and is a devastating condition usually requiring a hip replacement either primarily or later in life.
Diagnosis
Patients usually initially complain of a dull ache in the groin. As the condition progresses there is collapse and reactive inflammation, causing constant pain and eventually mechanical problems. The hip will become stiff and in advanced cases the collapse will cause leg shortening and giving way.
X-ray images of avascular necrosis in the early stages usually appear normal. In later stages it appears relatively more radio-opaque due to resorbtion of nearby living bone secondary to reactive inflammation. The necrotic bone itself does not show increased radiographic opacity, as dead bone cannot undergo bone resorption which is carried out by living osteoclasts. Late radiographic signs also include a radiolucent area following the collapse of subchondral bone (the "crescent sign") and ringed regions of radiodensity resulting from saponification with calcification of marrow fat (i.e. medullary infarcts).
Early diagnosis offers the chance of joint preservation, therefore all patients with unexplained hip pain should have an MRI scan. MRI findings are
There are many different methods for classification, often mixing symptoms and radiographic signs. The commonest are based upon the original x-ray methodology of Ficat-Arlet:-
Stage |
Symptoms |
Radiographs |
|
Early |
|||
0 |
Preclinical |
0 |
Normal |
I |
Preradiographic |
+ |
Normal |
II |
Pre-collapse |
+ |
Diffuse porosis, sclerosis, or cysts |
Transitional |
Flattening Crescent Sign |
||
Late |
|||
III |
Collapse |
++ |
Broken contour of head Sequestrum Joint Space Normal |
IV |
Osteoarthritis |
+++ |
Flattened contour Decreased joint space Collapse of the head |
This system did not quantify the extent of the condition and multiple extensions have been proposed. One example is the "Combined Necrotic Angle" proposed by Steinburg. To calculate, first the center of the femoral head is identified. Two lines are then drawn from this point to the borders of the lesion on both AP and Lateral radiographs. The sum of the angles on the AP and Lateral radiographs is the Kerboul angle. Lesions are classified as small, medium, or large:
|
|
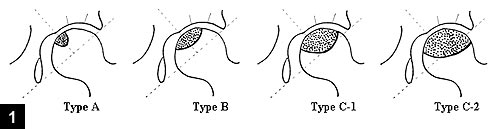
It is possible to annotated the location of the AVN based on the central coronal section of the femoral head on T1-weighted MRI images, as described by Nishii. Construct a perpendicular to a line from the acetabular edge and the tear drop (usually arising near the centre of the hip). The weight-bearing area is defined as the area lateral to the perpendicular.
Treatment
When this condition is discovered as an incidental finding and only affects a small proportion of the hip it is appropriate to simply observe. There are conflicting reports about the fate of these hips, however it is likely there are many more asymptomatic cases we never know about.
Pre-collapse
Once symptoms develop the natural history is always collapse and secondary arthritis, irrespective of stage or aetiology. A number of medical treatments have been tried to reduce the rate of collapse in early lesions:-
Statins: Pritchett et al published a retrospective review in 2001 that reported the incidence of osteonecrosis in 284 patients who had received high dose corticosteroids while concurrently on a statin. At 7.5 years follow-up MRI's were performed on all patients who complained of hip pain. Only 3 patients (1%) developed osteonecrosis which is significantly lower than the historical value of 5% for patients receiving high-dose steroids . A similar effect has been demonstrated in a rabbit study.
Bisphosphonates: A prospective, randomized, controlled trial has reported the results of 54 patients with large pre-collapse or early post-collapse lesions randomized either into a group that received observation only or a group treated medically with alendronate for 25 weeks. Seven percent (2/29) of the lesions treated with alendronate had progressed at a minimum 2-year follow-up versus 76% (19/25) of the controls.
Enoxaparin:Heparin has been reported to decrease disease progression in patients with an underlying thrombophilia and/or hypofibrinolysis and Stage I or II disease.
Core decompression was first described by Ficat and Arlet first in 1964 while investigating painful hips in patients who had normal radiographic findings. The theory of the procedure is to reduce intraosseous pressure in the femoral head, improving arterial inflow and potentially decreasing pain. A k-wire is drilled into the necrotic area under fluoroscopic guidance and is then over-drilled with a drill and trephine. Patients are kept partially weight bearing for six weeks to reduce the incidence of proximal femoral fracture through the drill hole (the main complication of this technique). This treatment is indicated for precollapse lesions with less than 30% involvement of the femoral head. A success rate of 84% for Stage I lesions and 65% for Stage II lesions has been reported.
A modification of this technique has been described and entails involves multiple percutaneous small drillings rather than one larger core, reducing the risk of fracture by avoiding a stress riser.
Another variation includes placement of a tantalum rod in the core tract. This technique theoretically provides subchondral support and decreases the risk of proximal femoral fracture by filling the cortical hole. Accurate placement of the device is key. The one or two studies published on this technique have shown comparable or slightly better results than those of standard core decompressions. Indications are same as for standard core decompression. If these patients eventually require a total hip arthroplasty, the tantalum rod will require removal.
Post-collapse
If there is significant collapse surgical treatment is indicated either head preservation or total hip replacement, depending upon the aetiology and the stage of the condition.
Head preserving operations aim to reconstruct the normal contour of the weight bearing articulation and prevent the development of arthritis. This will require removal of the dead bone and either; biological grafting to support the chondral surface, rotation osteotomy or artificial replacement of the damaged segment.
"Lightbulb" and "Trapdoor" procedures: may be used for post-collapse disease. These procedures require open dislocation of the hip to allow a window in the femoral neck or femoral head. The subchondral void is cleared of dead bone and packed with various types of bone graft perhaps with osteogenic factors. One study had reported a 83% success rate for patients with Stage III disease and 33% for those with Stage IV disease at a 4-5 year follow-up using the trapdoor procedure.
Arthrocap: There is interest in partial resurfacing with a stud of polished metal. This preserves the undamaged portion of the femoral head. At present this technique is not supported by any published studies.
Proximal femoral osteotomy: The rationale is to remove the necrotic or collapsing segment from the weight-bearing zone of the femoral head. This procedure should be considered in young patients with small to medium-size lesions (or a combined necrotic angle of less than 200). However an osteotomy can significantly complicate future conversion to THA due to the fact that anatomy is distorted and with retained hardware that can be problematic.
Vascularized bone grafting: The aim of this treatment is to introduce bone with it's own blood supply. In general, free vascularized fibular grafting is only considered for patients <35 years-old with pre-collapse lesions or those with collapse of <2mm. The procedure requires two teams, one prepares the proximal femur while the other harvests the vascularized fibula graft. The free fibula and cancellous bone graft are then inserted into a core tract and the peroneal vessels are joined to either the lateral circumflex artery or the ascending branch of the first perforator.
Patients are typically kept on protected weight bearing for 6 months. In addition to providing structural support, this procedure theoretically provides some amount of revascularization of the femoral head.
Results with this technique have been highly variable. Complications include donor site morbidity (24%) and proximal femur fracture (2.5%) . Lastly, conversion to total hip arthroplasty in patients who have undergone this procedure requires burring laterally to prevent the prosthesis from being misplaced.
Total hip replacement is by far the commonest treatment as it is effective and long lasting. Results are similar in patients of the same age who have hip replacement for other diagnoses.
© Mr Gavin Holt :: CotswoldClinics.com :: Print this frame